Abstract
Introduction: Use of cytoreductive therapy pre-transplant has remained a debatable issue in the management of MDS. Induction chemotherapy has been attempted with no clear advantage. However, the information on pre-transplant hypomethylating agents (HMA) as a debulking/bridging therapy in MDS is unclear. This study evaluates the impact of pre-transplant HMA on post-transplant outcomes in MDS.
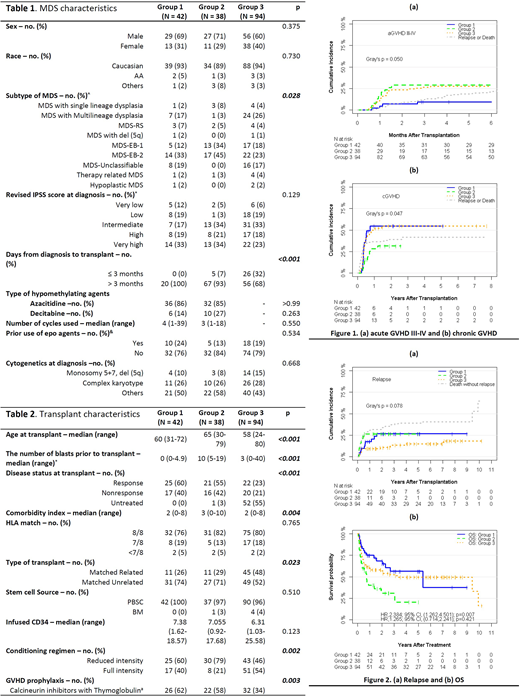
Methods: We retrospectively evaluated clinical outcomes of adult MDS patients, who underwent allogeneic stem cell transplant (ASCT) at out institute. We divided patients who received pre-transplant HMA into <5% blasts (group 1) and ≥ 5% blasts (group 2) at transplant and compared transplant outcomes of both these groups with untreated patients (group 3). The objectives were to determine rate of GVHD, non-relapse mortality (NRM), relapse rate, progression free survival (PFS) and OS.
Results: Between January 2000 and December 2016, 174 patients with MDS underwent ASCT. Of these, 80 patients received pre-transplant HMA, and 42 had <5% blast (group 1) and 38 had ≥ 5% blasts (group 2) at transplant. Ninety-four patients did not receive HMA (group 3). Monosomy 5, 7 or del 5q was noted in 10%, 8% and 15% of patients, in group 1, 2 and 3, respectively, whereas complex cytogenetics were noted in 26%, 26% and 28% of patients, in group 1, 2 and 3, respectively. Median number of blasts at transplant was 0%, 10% (range, 5-19), 3% (range, 0-40), in group 1, 2 and 3, respectively. Thirty-nine percent patients received matched related, and 61% received matched unrelated donor transplants. Bu-Flu-TBI (53%) was the most commonly used conditioning regimen followed by Bu-Flu (41%).
With a median follow up of 4.08 years, the cumulative incidence of grade III-IV aGVHD at 6 months was 9.5% (95% CI, 3-20.7%), 28.9% (95% CI, 15.5-43.9%), and 27.7% (95% CI, 19-37%) for group 1, 2 and 3, respectively (p=0.05). The 1-year cumulative incidence of cGVHD was 54.9% (95% CI, 37.4-69.4%), 28.4% (95% CI, 14.4-44.3%), and 51.1% (95% CI, 40.4-60.7%) (p=0.04), for group 1, 2 and 3, respectively. The 1-year OS for group 1, 2 and 3 was 75% (95% CI, 62.6-89.7%), 40.2% (95% CI, 26.5-61%), and 59.3% (95% CI, 50.1-70.1%), respectively; whereas PFS was 67.5% (95% CI, 54.4-83.8%), 34.8% (95% CI, 22.2-54.7%), 55.1% (95% CI, 45.9-66.2%), respectively. The 1-year outcomes in group 1, 2 and 3 were 17.6% (95% CI, 7.6-31%), 26.6% (95% CI, 13.6-41.6%), and 9.6% (95% CI, 4.7-16.6%) (p=0.07), respectively, for relapse; 14.8% (95% CI, 5.9-27.6%), 38.2% (95% CI, 22.4-53.9%), and 35.2% (95% CI, 25.7-44.9%) (p=0.11), respectively, for NRM. Multivariable analysis demonstrated that ≥5% blast at transplant, complex karyotype and high R-IPSS were associated with poor PFS and OS, whereas Complex karyotype was associated with higher relapse rate, poor PFS and OS.
Conclusion: Our study shows pre-transplant disease burden and complex karyotype as independent risk factors for poor outcomes. No survival benefit was noted with pre-transplant HMA in MDS.
Deol:Novartis: Consultancy; Kite Pharmaceuticals: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal